Cidara is developing targeted immunotherapies designed to save lives and improve the standard of care for patients facing serious diseases.
Targeted Immunotherapy
for Transformative
Outcomes
Targeted Immunotherapy
for Transformative Outcomes
Our Mission
Cloudbreak
Technology
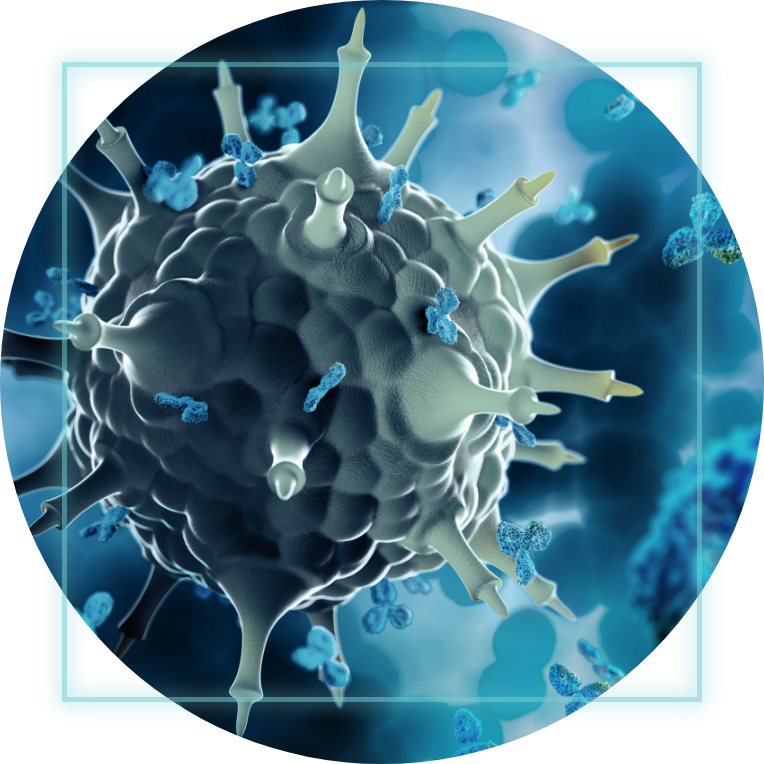
Our Cloudbreak platform creates “single molecule cocktails” by coupling targeted small molecules and peptides to a human antibody fragment (Fc). The resulting drug-Fc conjugate (DFC) immunotherapies are designed to inhibit specific disease targets while simultaneously engaging the immune system.


